It could be your mother, your brother, your best friend or your child who gets hurt at work. Can you imagine having your injured mom call on the phone to say her disability payment has not been received yet and the landlord is demanding rent payment? Or your young, injured son is confused and struggling to pick the right doctor, perhaps falling prey to an aggressive surgeon?
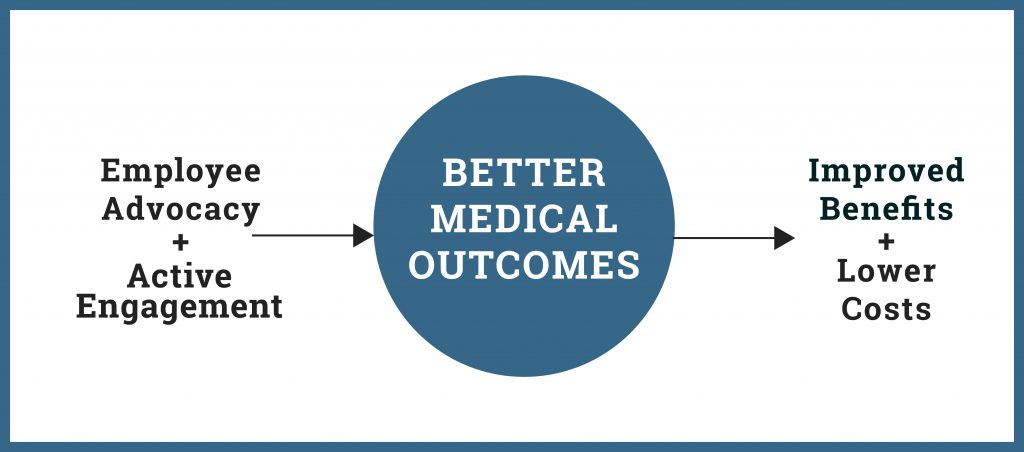
Families are impacted and livelihoods are at stake when injury occurs on the job. Pivoting from a decades-long emphasis on how to save more money on workers’ compensation, attention has shifted toward “employee advocacy” that makes these programs more user-friendly for a company’s most important asset: workers – and still reasonably controls costs.
An “employee advocacy claims model” within the workers’ compensation industry has not been clearly defined. Basically, it means two things:
- Good customer service that reduces complexity and demonstrates a “we care” attitude through early communication, respect, empathy and transparency toward the injured worker; and
- Creating a sense of urgency that active engages all key parties in the recovery process, without creating distrust by “hounding” the injured worker.
Specific examples include:
- Self-reporting of employee injuries through web, mobile (including text) and call center options.
- Greeting cards or other personal notes expressing care and a warm expectancy of return to work.
- Avoiding certain terminology, like “adjusting”, “examining” and “investigating”.
- Eliminating unnecessary paperwork for the injured worker.
- Delivering communications by electronic means to those workforces accustomed and well-equipped for it.
- Nurse case managers actively addressing emotional, family and other living condition issues, as well as actual medical management.
- Identifying and recruiting the best physicians, including those that do not normally accept workers’ compensation claims.
- Periodic contact with the injured worker (perhaps, by someone with no benefit claim decision-making authority) to see how they are doing and confirm understanding of the claim process.
- Hosting physician tours of the workplace to see injury exposures and modified duty opportunities.
- Demonstrating flexible approaches to return-to-work and a willingness to be creative and thoughtful about workplace or other job accommodations.
- Making benefit decisions and payments much sooner than the maximum time frames allowed by law.
- Direct deposits of disability checks into employee accounts, after any normal deductions for group health and retirement plan contributions, child support and union dues.
- When an injury benefit claim denial is appropriate, transitioning the worker to any other available employer-sponsored benefit programs (like a “warm referral” into a group health plan for non-work-related health conditions).
- Any other technique that supports the above two objectives for employee advocacy.
Many of these processes have been found in Texas injury benefit programs for 30 years. They are part of a constant pursuit of better medical outcomes and high employee satisfaction.
If you get that phone call from your injured mother or son, where can they turn for information? The front line in reducing complexity is a simple explanation of benefits BEFORE the injury occurs, with that information remaining available at any time. When paying medical and disability benefits outside of the Texas workers’ compensation system, federal law requires the employer to provide a summary plan description (SPD) to every worker upon hire. The SPD summarizes an official plan document that represents a contractual commitment by the employer to pay definitely determinable benefits. The SPD is commonly supplemented by a highlights brochure, employee hotline, and further simplified descriptions of available injury benefits and how they work. Paper or electronic copies of the SPD must remain available to employees at any time, and interpretive assistance is required.
Employee advocacy also requires continual quality improvement. Widespread updates to Texas injury programs have been made over the past three years to make them more user friendly, including:
- Removing unnecessary exclusions and limitations on coverage,
- Adding “good cause” exceptions for late injury reporting and medical management requirements,
- Ensuring the injury benefit program is the employee’s primary source of recovery, achieves better medical outcomes and pays more wage replacement (avoiding cost-shifting to government programs),
- Updates for new employee protections in ERISA disability claim regulations that became effective April 2, 2018, and
- More fiduciary training on claims handling to ensure a “full and fair review” – the legal standard approved by the U.S. Supreme Court for ERISA benefit claims.
Negligence liability exposure is also a powerful force for good. An employer’s loss of “Exclusive Remedy” protection can have an enormously positive impact on employee advocacy! Texas employers sponsoring injury benefit programs and their insurers would much rather promote good communication, safe workplaces and professionally-paid medical and disability benefits, than encounter disgruntled workers with damage claims for negligence that may have caused the injury. That’s one reason why these Texas programs pioneered employee advocacy techniques decades ago.

No Texas employer should simply “opt out” of workers’ compensation and fail to protect its injured workers. Gratefully, that behavior is far from the norm. Compared to other states that have a mandatory workers’ comp system, the Texas Department of Insurance reports a very high percentage (94%) of all Texas workers as having either workers’ compensation or injury benefit program protection.
To help workers know where their employer stands, the state maintains publicly available lists.
Employers not found on these lists are likely (and at a minimum) out of compliance with current Texas law reporting requirements, and should recognize that employee advocacy through workers’ compensation or a Texas injury benefit program is good for business.