By Jeff Pettegrew
This year’s National Workers’ Compensation and Disability Conference and Expo in Las Vegas – the country’s biggest workers’ comp conference – was filled with learning and networking opportunities as well as an exhibit hall packed with the latest and greatest innovative products and services. Take a look at some of my highlights from the conference!
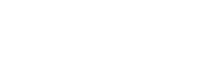
NOVEMBER 6TH: GUEST SPEAKER, DR. DREW PINSKY
Dr. Drew Pinsky, Addiction Specialist, Doctor of Internal Medicine & TV personality was the opening Keynote covering the topic: “The Pitfalls and Challenges in Treating the Addicted Patient.” Dr. Pinsky indicates that we need to understand what addiction is, how it’s amplified, and how to identify and correct it.
He began with an amazing, informative 200 year history of the use of opioids wherein little evidence was ever sought to refute the addictive outcome using these types of drugs. Opiates were commonplace treatments.
“The goal,” he said, “should be a return to a flourishing life and not chronic illness and not disability. A return to a flourishing life.”
He noted: “There is no way than an orthopedist or pain management doctor or even many psychiatrists can manage them. There’s also a massive shortage of psychiatrists in general, particularly psychiatrists who can really handle cases like this.” Adding to the challenges, he says the biggest mistake that everyone makes, particularly if you’re dealing with an addict, is believing them. Malingering is a common attribute. Everything has to be objectively measured. 60% of addiction is genetic.
Dr. Pinsky emphasized that we should be aware that someone who is depressed is distracted and will be more likely to get injured. Interestingly, Buprenorphineh noted, is a new drug that has the potential of treating addiction to opioids.
Most importantly, a proper and thorough diagnosis is critical due to the complexity of pain management. He closed by saying: “A flourishing life should be our goal.”
NOVEMBER 6TH: THE MEDICAL IMPERATIVE

Progressive Strategies for Cutting Costs” with panelists Denise Alguire, Albertson’s, Brian Trick, Wegman’s Food Markets, and Kim Haugard, Texas Mutual Insurance.
Medical management is a complex process involving claims examiners and medical professionals.
Workers’ Compensation, as Denise Alguire stated, is truly a benefit delivery system.
Examine the frictional components and unnecessary delays of workers’ comp claims management system. Too much red tape and supervisorial delays? Some organizations, like Starbucks, are using employee self-reporting of workplace injuries. The injured worker has to fill out the details of an accident or injury and file it immediately versus waiting for a formal claims adjuster’s recorded phone interview. Follow up post-accident workplace safety reviews and loss prevention efforts are a critical component as well. Ironically, employers with self-reporting report a reduction in denied claims as a result. It’s an incentive to be honest and accurate.
Other lifestyle issues like comorbidities such as obesity and hypertension can impact costs and outcomes of workplace injuries by factors of 7 to 10 times normal. Worker stress, often from non-work issues, is an important factor to address. In addition, aging workers create increased health hazards that employers should be cognizant of.
Having loved ones or family members accompany the injured worker to medical treatment is a very positive influence on solving associated psycho-social risk factors and issues and works to reduce stress and distrust factors.
Promoting physical and mental health and wellness is also a key employer-provided program to educate workers in a number of helpful ways both before and after workplace injuries.
Maximum medical improvement (MMI) is a functional term, but it should never be the ending if a claim. Never give up trying to get the injured worker healthier and more productive. In that light, medical provider quality, outcomes, and personal performance on your behalf – as reflected in benchmarking efforts – are of great importance. Value based payment models are often used instead of the out of vogue discounted fee models. Simply put, injured workers should be channeled to the highest and best medical performers. Their outcomes are the critical factor.
Furthermore, treating physicians that have caring attitudes and provide personal encouragement to injured workers are key.
They can be helpful in identifying things outside of employment that can benefit the worker or his/her family at home.
Also, workers appreciate understandable medical and benefit terminology as opposed to workers’ comp terms and technical jargon. Devote more effort toward employee advocacy, and use teams of experts, as necessary, to speed up and streamline the claims approval process.
In areas of wellness, Wegman’s Food Markets, for instance, uses L.A. Fitness to provide employer sponsored health and exercise fitness facilities and programs.
The panel concluded their remarks emphasizing the importance of leveraging useful data and innovative advanced technology, including mobile apps, to help achieve better outcomes. Using mail or phone calls to communicate, as an example, is typically outdated and ineffective.
Injured worker focus groups is another great way to evaluate and improve your program’s effectiveness. Most importantly, the quality of life outside work is an important ingredient to better outcomes. The mantra of a successful workers’ comp program is to strive for “Quality of Life” decision making.
NOVEMBER 7TH: AWARD-WINNING EMPLOYERS SHOWCASE THEIR SUCCESSFUL WORKERS’ COMP STRATEGIES
Laurie Frey, Kohl’s; Brett Jeziorski, City of Surpise, AZ;John Madaus, Clemens Food Group; Joe Molloy, Northwell Health; and Brad Waldron, Caesar’s Entertainment.
This diverse group of workers’ comp experts shared their award-winning strategies in a lively interchange of ideas and accomplishments. Innovative concepts included:
- Employer sponsored wellness centers with personal trainers to help reduce a wide range of co-morbidities and addictions. Kohl’s actually allows family members to participate
- Targeted on-site training of TPA claims examiners to understand work environment and culture
- “Wait and see” is not an effective strategy
- Ensure that TPA and other intermediaries treat injured workers with respect and kindness
- Provide treating physicians with a detailed description of modified duty opportunities and their physical demands
- Behavioral safety is teaching employees watch out for each other – use the buddy system when needed
Develop Return-to-Work teams (usually HR) to enhance employee advocacy and better outcomes vs. relying on the worker’s supervisors to work it out - Provide meaningful feedback to assigned medical teams to share challenges and success stories
- Allocating some portion of workers comp company expenses based upon each unit’s frequency/severity experience encourages accountability
- Keep supervisors and management informed of your injury benefit and safety program goals and results
- Survey injured workers after claim resolution to evaluate WC program needs and effectiveness – a live interview is far better than a form.
- Some of the panel members do NOT use nurse case managers based upon trial and error experience – “partner relationships” are preferred
- Report all incidents and your team should take it from there to figure out what follow-up strategies are desired
- Avoid using “claim” or case numbers with injured workers and focus on medical improvement and return-to-work
NOVEMBER 7TH: SCOTT DANIELS, ESQ., COMCAST NBC UNIVERSAL
Managing over 200,000 diverse employees nationwide, Mr. Daniels covered the various aspects of paid and unpaid disability from workers’ comp to STD, LTD, FMLA and bereavement leave.
With various applicable state and federal laws, compliance standards, and rule complexity, this wide combination of legal disability rights of the workforce is very complicated. He asserts: “Prepare to see more health and disability leave usage.” Employees are seeking more flexibility in planned and unplanned work absences.
In some cases, several programs may overlap. In addition, various workforce members with age and health variances desire different types of benefits. One size does not fit all, and this means various vendors are utilized to manage these various leave programs. A cohesive approach is a challenge.
The rapid growth of a gig economy creates additional demands as workers want to remain flexible. It’s becoming an on-demand world and there is increasing awareness of these workplace benefits by employees whether the situations are work-related or not.
The biggest factors impacting absence management includes 6 key areas:
(1) analytics
(2) technology
(3) communication
(4) employee population
(5) health, and
(6) business evolution.
Comcast takes disabled field technicians, as an example, and uses them in their traditional service center locations.
The delivery of benefits needs to address employee advocacy via value-based designs that build opportunities to return employees to work. Digital tools are very helpful ways of communicating. This also involves vendor collaboration to make sure your objectives are well aligned.
Analytics need to understand usage and trends to track the ever-changing needs of your workers as job descriptions and the work environment and the workforce changes. You also need to understand the whole breadth of eligible benefits.
NOVEMBER 7TH: “THE OPTIMIZED PATIENT” V.I.P. BOOK SIGNING EVENT
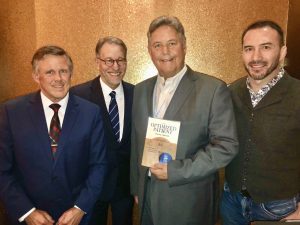
To my far right is outdoorsman, Doug Anend. Immediate right is the book author and L.A. tv personality, Harvey Warren. To my left is Nathan “Rock” Quarry – a retired world renown martial arts fighter and champion from The Ultimate Fighter.
All suffered life threatening injuries and surgeries, but benefited and recovered dramatically from natural, simple lifestyle changes before and after life altering surgeries.